Fix Inefficiencies in Claims Process
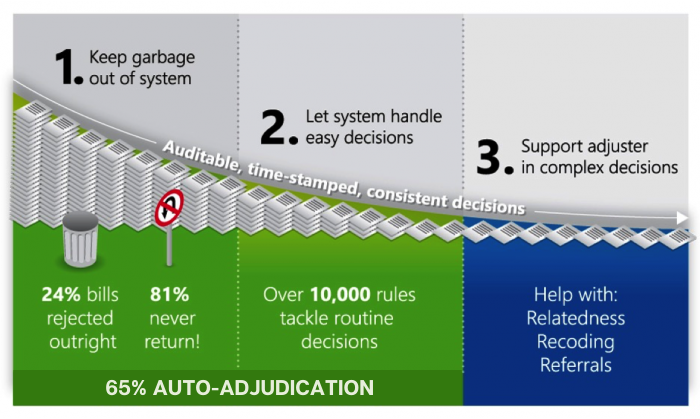
Our automated systems streamline routine documents by preventing human error and reducing time-consuming costs by auto-adjudicating up to 65% of incoming documents and recognizing over 130 form types. In short, we save you from paying unrelated and duplicate bills.
APS Systems Auto-Adjudicate Up to 65% of Incoming Documents
Streamline the Routine Documents
Keep Garbage Out of Your System
Interested in Learning More?
Reduce Medical Loss
Our clients typically improve medical loss by 11 points, with some seeing up to a 23-point improvement.
Our automated and integrated claims system significantly reduces medical loss by examining and verifying claims every step of the way to prevent over-payment and leakage. Only verified documents are routed to the correct review process, which eliminates costs associated with unauthorized services.

Drop Medical Loss
Eliminate Claims Leakage and Overpayment
We typically reject up to 32% of bills from the beginning, and 58% of those never get returned. You won’t pay for unrelated bills anymore.
Gain Control Over Your Provider Networks
Make changes to provider networks easily
Network Transparency
Easy Onboarding of New Partners
Problems We Solve/Increase the Power of Your Adjusters
APS automates the easy tasks, giving adjusters 40% more time to focus on the complex decisions.
On average, workers’ compensation adjusters manage 130 open cases, 20 bills from 6 different providers, 20 additional documents per claim, and are required to stay on top of 7,800 CPT codes and 68,000 ICD-10 codes. That’s a heavy load for even the most successful adjuster.
Our systems automate the easy, yet error-prone, tasks that take up a majority of an adjuster’s time. By improving efficiency, we allow them to focus on solving the difficult decisions they were trained and hired to do.

Reduce Human Error, While Keeping Sound Judgement Intact
Just How Busy Are Adjusters?
APS surveyed workers’ compensation adjusters and found that their workload averages….
130 open cases
20 bills from 6 different providers, and 20 additional documents per claim
7,800 CPT codes and 68,000 ICD-10 codes to stay on top of

